I understand you’re looking for an incredibly detailed and personalized guide on how to care for someone after knee replacement surgery. This is such a thoughtful and crucial role, and I’m here to equip you with all the knowledge and empathy you’ll need to support your loved one through this transformative journey, especially when considering Total Knee Replacement Surgery in India.
Caring for someone after total knee replacement surgery is a profound act of love and commitment. It’s about being their anchor, their cheerleader, and their practical support system as they navigate the path to renewed mobility. Let’s delve deep into the art of caregiving, providing you with a comprehensive understanding of what to expect and how to make this period as smooth and successful as possible.
Your Guiding Hand: 10 Essential Tips for Caring for Someone After Knee Replacement Surgery
My dear friend, you are about to embark on a vital role in someone’s life – that of a primary caregiver after their total knee replacement surgery. This isn’t just about fetching things; it’s about providing emotional support, practical assistance, and unwavering encouragement. Your efforts will significantly impact their recovery journey, making a world of difference. So, let’s explore these 10 tips that will empower you in this crucial role.
Tip 1: Be Prepared – Knowledge is Your Superpower

Before your loved one even steps into the hospital for their total knee replacement surgery in India, your preparation can make a world of difference. This isn’t just about gathering supplies; it’s about understanding the journey ahead.
Educate Yourself:
- Understand the Procedure: While you don’t need to become a surgeon, having a basic understanding of what happens during total knee replacement surgery will help you grasp the “why” behind the recovery protocols. Many hospitals, including those in India, offer pre-operative classes or materials for patients and their families. Attend these if possible.
- Anticipate the Recovery Timeline: Know that recovery is a marathon, not a sprint. While initial progress might be rapid, full recovery can take several months to a year. Managing your expectations will help you manage theirs.
- Learn About Potential Complications: Being aware of signs of infection, blood clots, or other issues (like increased pain, redness, swelling, fever, or shortness of breath) means you can act quickly if they arise. This knowledge isn’t to scare you but to empower you to be vigilant.
Prepare the Home Environment:
- Clear Pathways: Walk through every room your loved one will use. Remove throw rugs, loose cords, or any clutter that could cause a trip or fall.
- Bathroom Safety: Install grab bars in the shower and next to the toilet. A shower chair and an elevated toilet seat are invaluable for safety and ease of use.
- Bedroom Accessibility: Ensure their bed is at a comfortable height for getting in and out. If stairs are an issue, consider setting up a temporary sleeping arrangement on the ground floor.
- Essentials within Reach: Place frequently used items – water, medications, tissues, remote controls, books, phone – on a bedside table or in an easily accessible spot to minimize stretching or bending.
- Consider Assistive Devices: Crutches, walkers, and reaching aids might be needed. Ensure they are readily available and in good working order.
Logistical Planning:
- Meal Prep: Cook and freeze meals in advance, or plan for easy-to-prepare options. You’ll be busy, and nutritious food is essential for healing.
- Transportation: Arrange for transportation home from the hospital and for follow-up appointments.
- Support System: Identify other family members or friends who can offer assistance, whether it’s running errands, cooking, or just providing a break for you.
Ensure a faster, smoother recovery after knee replacement—book an expert consultation today!
Book AppointmentTip 2: Master Pain Management – Be Their Advocate
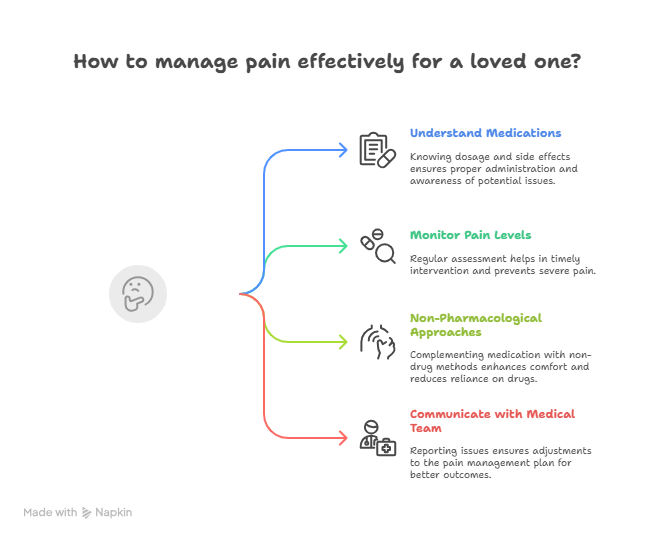
Pain control is paramount in the initial stages of recovery. Uncontrolled pain can hinder participation in physical therapy, delay progress, and cause immense distress.
Understand Their Medications:
- Pain Relievers: Your loved one will likely be prescribed a combination of pain medications, including opioids for acute pain and potentially NSAIDs or acetaminophen for less severe discomfort. Understand the dosage, frequency, and potential side effects of each.
- Other Medications: They may also have blood thinners (to prevent clots) and possibly antibiotics. Ensure you know the schedule for all medications.
- Side Effects: Be aware of common side effects like constipation (especially from opioids – ensure they have a stool softener or laxative if needed), nausea, or drowsiness.
Monitor Pain Levels Diligently:
- Ask Regularly: Don’t wait for them to tell you they’re in pain. Ask them frequently about their pain level using a 0-10 scale. This objective measure helps you understand their needs.
- Timely Dosing: Administer pain medication on schedule, even if they claim they’re not in severe pain at that moment. Staying ahead of the pain is much easier than trying to catch up once it’s severe.
- Non-Pharmacological Approaches: Incorporate non-drug methods like ice packs (follow instructions for application – usually 20 minutes on, 20 minutes off), elevation of the leg, and gentle repositioning. Distraction (music, reading, conversation) can also be effective.
Communicate with the Medical Team:
- Report Inadequate Pain Control: If their pain is consistently high despite medication, don’t hesitate to contact their surgeon or nurse. Their pain management plan may need adjustment.
- Document: Keep a simple log of medication times and pain levels. This information is invaluable for discussions with the medical team.
Ensure a faster, smoother recovery after knee replacement—book an expert consultation today!
Book AppointmentTip 3: Champion Physical Therapy – Your Unwavering Support
Physical therapy is the cornerstone of recovery after total knee replacement surgery. Your role here is critical.
Encourage and Motivate:
- Consistency is Key: Emphasize that performing the prescribed exercises regularly, even when tired or slightly uncomfortable, is non-negotiable for a successful outcome.
- Gentle Nudges, Not Demands: Avoid being overly pushy. Instead, frame it as a partnership. “It’s time for your exercises, how about we do them together?”
- Celebrate Small Victories: Acknowledge every bit of progress, no matter how small – a slightly better bend, an extra step, less pain during an exercise. Positive reinforcement is powerful.
Assist with Exercises:
- Learn the Routine: If possible, attend physical therapy sessions with your loved one so you can learn the correct form and technique for each exercise.
- Provide Support: Help them with positioning, provide a steadying hand, or count repetitions.
- Monitor for Pain/Discomfort: Watch for signs of excessive pain during exercises. While some discomfort is normal, sharp or increasing pain warrants a break and possibly a call to the physical therapist.
Facilitate Sessions:
- Transportation: Ensure they get to and from their therapy appointments.
- Comfort: Make sure they are comfortable before and after sessions, with access to ice or pain relief.
Tip 4: Monitor for Complications – Be Vigilant and Proactive
Being aware of potential issues allows you to seek timely medical attention, which can prevent more serious problems.
Signs of Infection:
- Redness or Swelling: Increased redness around the incision site, or new/worsening swelling.
- Warmth: The skin around the incision feeling unusually warm to the touch.
- Pus/Drainage: Any discharge from the incision that is cloudy, yellowish, or foul-smelling.
- Fever: A temperature over 101°F (38.3°C) or chills.
- Increased Pain: New or worsening pain at the incision site.
Signs of Blood Clot (Deep Vein Thrombosis – DVT):
- Calf Pain: New pain in the calf or thigh that doesn’t go away.
- Tenderness: Tenderness to touch in the leg.
- Swelling: New swelling in one leg (compared to the other).
- Redness/Warmth: Redness or warmth in the affected leg.
- Seek immediate medical attention if you suspect a DVT.
Other Concerns:
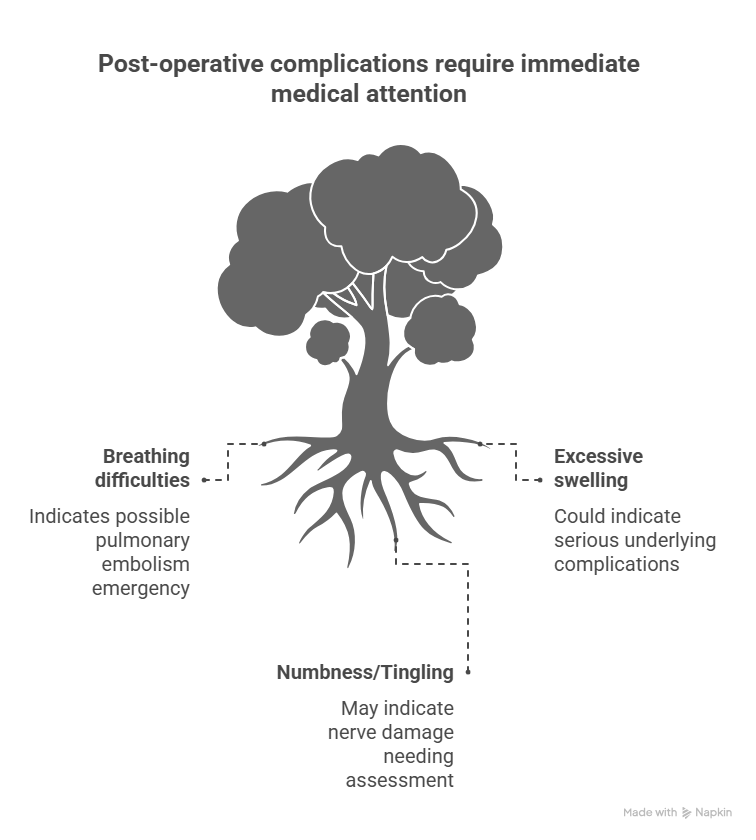
- Shortness of Breath or Chest Pain: These could indicate a pulmonary embolism (a blood clot that has traveled to the lungs) – a medical emergency. Call emergency services immediately.
- Excessive Swelling: While some swelling is normal, if it’s severe, persistent, or accompanied by other symptoms, contact the doctor.
- Numbness/Tingling: While some temporary numbness around the incision is normal, report any new or worsening numbness or tingling in the foot or toes.
Communicate with Impact Ortho: Don’t hesitate to call the team at Impact Ortho if you have any concerns whatsoever. They are your primary resource for medical advice.
Ensure a faster, smoother recovery after knee replacement—book an expert consultation today!
Book AppointmentTip 5: Assist with Daily Activities – Practical Support
In the initial weeks, your loved one will need significant help with basic tasks.
- Bathing and Dressing: Help them shower (using a shower chair for safety), and choose loose-fitting, comfortable clothing that is easy to put on and take off. Adaptive dressing aids might be helpful.
- Toileting: Assist with getting on and off the toilet, especially if an elevated seat is not used.
- Meal Preparation: Prepare nutritious meals that are easy to eat. Ensure they are hydrated with plenty of water.
- Mobility Assistance: Help them transfer from bed to chair, and walk with them using their assistive devices, providing a steadying arm.
- Medication Reminders: Ensure they take their medications on time.
Tip 6: Manage Swelling and Bruising – Comfort Measures
Swelling and bruising are common after total knee replacement surgery, but you can help manage them.
- Elevation: Encourage them to keep their leg elevated above heart level whenever possible, especially when resting. Use pillows to prop up the leg.
- Ice Packs: Apply ice packs to the knee for 15-20 minutes at a time, several times a day. Ensure there’s a thin cloth barrier between the ice and the skin to prevent frostbite.
- Compression: Follow your surgeon’s instructions regarding compression stockings or bandages.
- Gentle Movement: Regular, gentle ankle pump exercises (flexing and pointing the foot) can help reduce swelling by improving circulation.
Tip 7: Nurture Their Mental and Emotional Well-being – Beyond the Physical
Recovery is as much a mental game as it is physical. Your emotional support is invaluable.
- Patience and Empathy: Understand that they will have good days and bad days. Some days they might feel frustrated, discouraged, or even tearful. Acknowledge their feelings without judgment. “It’s okay to feel frustrated, this is a tough process, but you’re doing so well.”
- Encourage Independence (Gradually): While you’re there to help, encourage them to do what they can safely do for themselves, even if it takes longer. This fosters a sense of accomplishment and rebuilds confidence.
- Keep Them Engaged: Avoid isolating them. Encourage them to engage in light activities they enjoy, such as reading, watching movies, listening to music, or gentle conversation.
- Celebrate Progress: Point out the improvements you see, no matter how small. “Look how much further you bent your knee today!”
- Maintain a Positive Environment: Your positive attitude can be contagious. Try to keep the atmosphere light and hopeful.
- Listen Actively: Sometimes, they just need to vent. Listen without trying to fix everything.
Tip 8: Prioritize Your Own Well-being – You Can’t Pour from an Empty Cup
This is arguably one of the most overlooked, yet critical, tips. Caregiving can be physically and emotionally draining.
- Ask for Help: Don’t try to do everything yourself. Delegate tasks to other family members or friends. Accept offers of help.
- Take Breaks: Schedule time for yourself, even if it’s just 30 minutes to read, take a walk, or simply sit quietly. You need to recharge.
- Maintain Your Own Health: Eat well, get enough sleep, and try to incorporate some physical activity into your routine.
- Communicate Your Needs: Talk openly with your loved one (when they’re feeling up to it) about your own needs and limits.
- Seek Support: If you’re feeling overwhelmed, talk to a trusted friend, family member, or consider joining a caregiver support group. Remember, you’re doing an amazing job, but you need care too.
Ensure a faster, smoother recovery after knee replacement—book an expert consultation today!
Book AppointmentTip 9: Facilitate a Healthy Diet and Hydration – Fuel for Healing
Proper nutrition is essential for wound healing, muscle repair, and overall recovery.
- High Protein: Lean proteins (chicken, fish, eggs, lentils, dairy) are crucial for tissue repair.
- Fruits and Vegetables: Provide essential vitamins, minerals, and antioxidants to support the immune system and reduce inflammation.
- Whole Grains: Offer sustained energy.
- Fiber: Crucial to prevent constipation, a common side effect of pain medications and reduced activity. Ensure they consume plenty of fiber-rich foods and consider a stool softener if needed.
- Stay Hydrated: Encourage frequent sips of water throughout the day. Dehydration can lead to fatigue and constipation.
- Avoid Processed Foods and Sugary Drinks: These offer little nutritional value and can contribute to inflammation.
Tip 10: Plan for Long-Term Support – The Marathon Continues
While the most intensive caregiving period might be the first few weeks, your support will be needed for months to come.
- Continued Encouragement for Exercise: Reinforce the importance of continuing their home exercise program long after formal physical therapy ends.
- Gradual Return to Activities: Support their gradual return to hobbies, social activities, and work. Don’t rush them, but encourage progressive engagement.
- Listen to Their Body: Teach them to listen to their new knee. If they experience pain or swelling after an activity, it’s a sign to ease off.
- Follow-Up Appointments: Ensure they attend all follow-up appointments with their surgeon at Impact Ortho. These appointments are crucial for monitoring long-term progress and addressing any concerns.
- Be a Long-Term Partner: Remind them that you’re there for the long haul, celebrating their milestones and offering support through any challenges.
Ensure a faster, smoother recovery after knee replacement—book an expert consultation today!
Book AppointmentFAQs: Addressing Your Concerns as a Caregiver After Total Knee Replacement Surgery in India
As a caregiver, you’re bound to have many questions. Here are some common ones that arise when supporting someone after total knee replacement surgery in India:
How long will my loved one need my full-time assistance?
The most intensive period of full-time assistance typically lasts for the first 1-3 weeks after discharge from the hospital. During this time, they’ll need significant help with personal care, mobility, and medication management. After this, their independence will gradually increase, but they will still benefit from your support for several weeks or even months with tasks like driving, heavier chores, and ensuring they stick to their physical therapy.
What are the signs that my loved one is overdoing it with their exercises?
Signs of overexertion can include increased or persistent pain (beyond the expected post-exercise soreness), significant new swelling, increased warmth around the knee, or excessive fatigue that lingers. Encourage them to listen to their body and communicate any new or worsening symptoms to you and their physical therapist. A little soreness is normal, but sharp pain or significant discomfort should prompt a rest.
When can my loved one start driving again?
This varies, but generally, a person can start driving approximately 4-6 weeks after total knee replacement surgery, provided it’s their right knee (for automatic cars) and they are no longer taking strong opioid pain medications. If it’s their left knee in an automatic car, they might be able to drive sooner. They must have good reaction time, adequate strength to operate pedals, and sufficient range of motion. Always get clearance from their surgeon at Impact Ortho before they resume driving.
How do I help them sleep comfortably at night?
Sleeping can be challenging initially. Encourage them to sleep on their back with their leg elevated on pillows (to reduce swelling). They can also try sleeping on their side with a pillow between their knees. Applying ice before bed and ensuring they take their pain medication on schedule can help promote comfort and better sleep. Gentle stretching before bed can also sometimes ease stiffness.
What is the role of nutrition in their recovery, and how can I help?
Nutrition is incredibly important! You can help by preparing balanced meals rich in protein (for tissue repair), vitamins, and minerals (found in fruits and vegetables for healing and immunity). Ensure they are drinking plenty of water to stay hydrated and to help prevent constipation, which is common with pain medications. Limiting processed foods, excessive sugar, and unhealthy fats can also support their overall healing.
When should I encourage them to start walking without assistive devices?
This decision should always be guided by their physical therapist and surgeon. They will gradually progress from a walker to crutches, then to a cane, and eventually to walking independently. Rushing this process can lead to falls or injure the new knee. Your role is to support the therapist’s recommendations and provide a safe environment for their progression, never pushing them beyond what the professionals advise.
Caring for someone after total knee replacement surgery in India is a journey of patience, love, and practical support. Your dedication will be instrumental in their return to an active and pain-free life. Remember, the team at Impact Ortho is always there to provide expert guidance and support to both the patient and you, the dedicated caregiver. You are an unsung hero in this recovery, and your efforts are truly invaluable. Impact Ortho applauds your commitment.











